
A 'dead' CRISPR might be a better CRISPR for targeting Alzheimer's
A new molecular editor based on "dead Cas9" shows encouraging results for editing the genome
The CRISPR genome editing revolution began almost a decade ago, and is almost old hat by now. But, when a group led by Professor Jonathan Weissman aimed to silence a gene involved in the progressive neurodegeneration seen in Alzheimer’s disease, they looked to different tools in the CRISPR toolbox. They developed their own version of a CRISPR genome editor that they named “CRISPRoff.”
CRISPR allows scientists to perform genome editing at any gene, in any desired species, with just two components. The first is an enzymatic protein called Cas9 — the molecular scissors. The Cas9 element gets close to the DNA's double helix, creating cuts in the DNA. Eventually, these cuts are healed by the cell, but they are healed in a non-perfect way, resulting in a “mutation” in the gene.
To ensure that the Cas9 cuts in a specific place and not randomly across the genome, it needs to be paired with a homing-device-like molecule called a single guide RNA. That RNA's specificity allows scientists to mutate their gene of interest, disrupting its activity in order to study its function in different cell types or species.
However, this strategy carries a risk. Studies have shown that the types of mutations occurring at genes can be too large: When large portions of DNA get deleted, it is challenging to know how far along the chromosome this deletion actually stretches. The type of mutation occurring can also be unpredictable or variable between individuals or cell types. Or it may be highly complex, resulting in DNA segments being rearranged or flipped within the chromosome.
Now, instead of cutting DNA, newer methods of controlling gene activity could beat Cas9 at its own game. This is particularly important in clinical trials where the required outcome always needs to be predictable and consistent, something traditional CRISPR frequently can't do. This new approach uses a molecule called dead Cas9 (dCas9) which does not create mutations in the DNA to kill the gene, but rather causes them to be silenced. Researchers have used dCas9 to permanently reduce the activity of a gene called MAPT, which has been implicated in Alzheimer's disease.
If Cas9 is a molecular scissor, then dead Cas9's scissors are completely blunt. So, when dragged to the target gene by the homing RNA, dCas9 cannot cut DNA. Instead, it sits on top of the DNA sequence, functioning like a genetic roadblock, preventing activity without creating mutations. Imagine that you were trying to drive your car out of a parking space, but a lorry parked directly in front of your exit, preventing you from moving.
To make the silencing process more efficient — essential for use in a clinical trial — researchers fused dCas9 to multiple other proteins, the most critical being methyltransferases. Methyltransferases create chemical modifications on the DNA by depositing a chemical group directly to the DNA strands, in a process called “DNA methylation.” DNA methylation is a naturally occurring chemical modification, also known as epigenetic modifications. And CRISPRoff is an epigenetic genome editor.
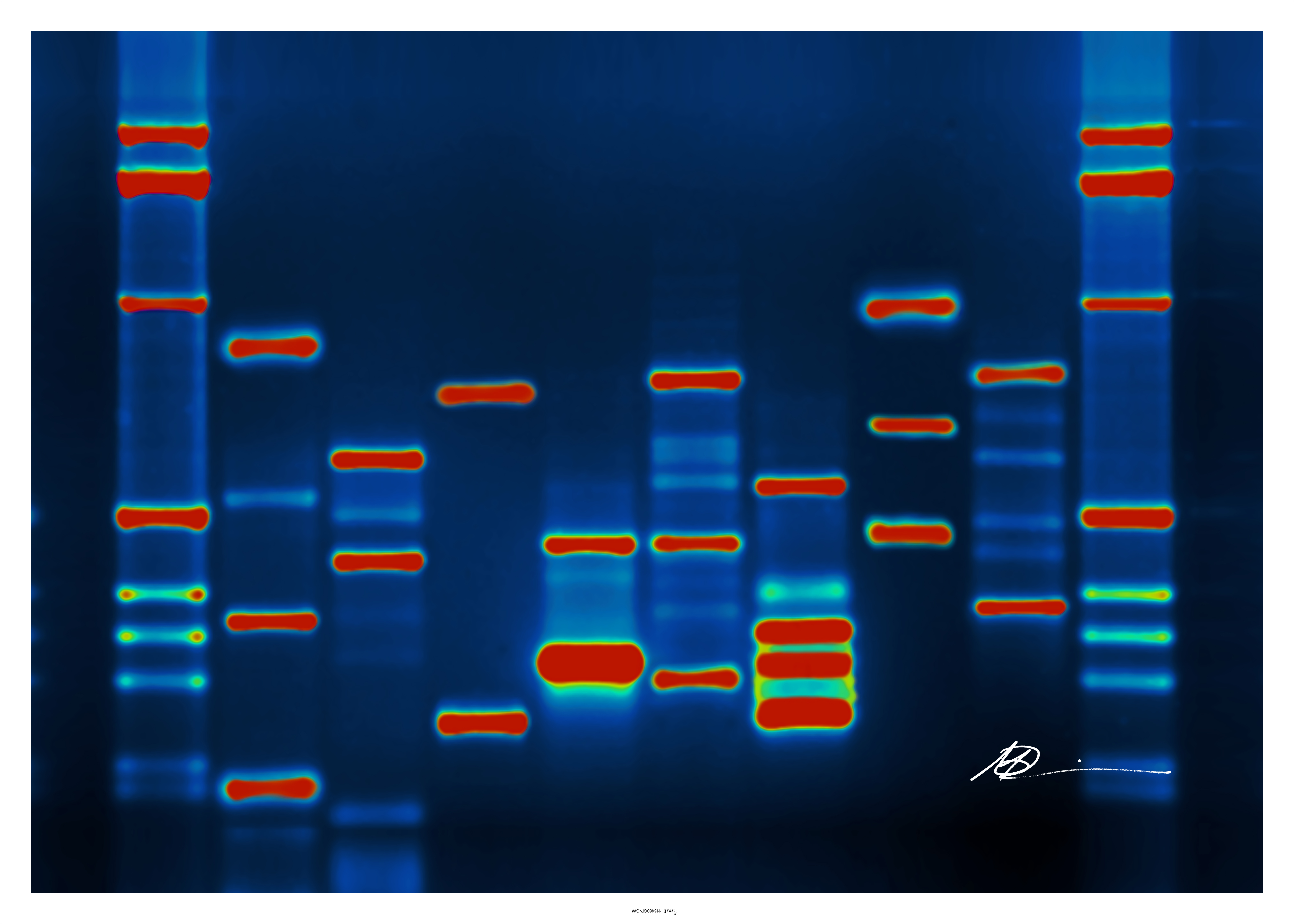
Micah Baldwin via Flickr
To test CRISPRoff before going to the clinic, Weissman's group introduced their dCas9 and attached molecules into a dish of cells engineered to glow green. After introducing CRISPRoff with a homing RNA to target the "green gene," they found that the green cells lost their color. This observation told the researchers that the silencing was working. Not only this, but they found that even when the dCas9-methyltransferase fusion was no longer visible in the cells, the silencing remained.
This permanent silencing was an important breakthrough. Previous experiments with dCas9 without fused methyltransferases had found that although dCas9 alone can block gene function for a short time, eventually the block fades, and the gene that was silenced can become reactivated. (It's as if the lorry eventually rolls away downhill, no longer blocking your exit.)
This meant if dCas9 was to be used for a clinical trial, the molecules may have to be continually replenished, which could introduce some side effects in participants.
The group then introduced CRISPRoff into human stem cells in a dish, targeting the gene MAPT. Active MAPT produces the protein tau, which has been often implicated in the progression of Alzheimer’s disease. By inhibiting the activity of this gene and thereby reducing tau levels, it is possible that neurodegeneration could be slowed down. They found that tau protein levels were reduced by around 30 percent. Moreover, they induced the stem cells to transform into neuron-like cells in a dish. In these neurons, they found that the silencing was maintained, indicating that CRISPRoff works even through cell divisions and differentiation.
On top of successfully silencing genes, the Weissman group produced the "antidote" to their CRISPRoff strategy, calling it CRISPRon. By adding CRISPRon to the cells, they are able to remove the DNA methylation, switching the gene back on.
Although the results of this study have potentially great benefits for translating to a clinical trial using CRISPRoff, there are still limitations for use in the human body. The CRISPRoff system — dCas9 and attached molecules — is a very large protein complex. Although it is currently simple to add this complex into human cells grown in a dish, it's much harder to package it into a vector that gets into the body. And although the results of these experiments silencing MAPT were consistent and long-lasting, it is not yet known whether this would be recapitulated as efficiently in people. It will be vital to ask questions about how to deliver and maintain the CRISPRoff system in the body.
