
Photo by Kristaps Grundsteins on Unsplash
Scientists can diagnose skin diseases like eczema with tiny zaps of electricity into your skin
But you won't feel it; 225 small, small pins can diagnose damage by specific skin layer
Our skin is a flexible fortress, defending our bodies from the outside world. But not everyone’s fortresses are created equal. Some people, like those with eczema, have less effective, disrupted skin barriers. Eczema is more common in children, but it’s estimated that up to 10% of people are affected by it during their lifetime. In the skin of those who live with eczema, germs and allergens can infiltrate more easily, causing local inflammation and chronic flare ups that can impact a person physically, emotionally, and socially.
Despite its prevalence, there is no test for eczema. Those who have it often find out only when they start to get flare ups. Even in the absence of visible flare ups, the skin of people with eczema is less functional. The good news is that defective skin can be identified with the right tool. Unfortunately, the tool currently in use, which measures transepidermal water loss (TEWL), is not very reliable. TEWL is a measurement of the amount of water leaving the skin over a period of time. Preventing water loss is an important function of skin, so those with fully functional skin will lose less water than those with dysfunctional skin over the same time period. However, measurements using TEWL can be impacted by the time of year, humidity, temperature, and even skin hydration levels. Therefore, we need a better tool to test skin function.
Scientists at the Swiss Institute of Allergy and Asthma Research in Switzerland recently tested a new tool, called Electrical Impedance Spectroscopy (EIS), for its ability to detect disrupted skin barriers. EIS works by measuring the flow of small, harmless pulses of electricity through materials like body tissue. Tissues like the skin are composed of many cells of differing types, shapes, and sizes. The electrical pulses will flow freely if nothing is in the way, but the tissue will impede that flow in different ways. Greater resistance to flow correlates with greater skin barrier function. The EIS device that the researchers used contains an ultrasensitive electrode, composed of 225 miniscule pins. Importantly, the device is both lightweight and portable, and the procedure is quick and non-invasive, making EIS a good candidate for measuring skin function, especially for individuals with sensitive skin.
EIS is not a new technology and different forms of it are already in use for other medical applications. The electrical impulses can detect differences in tissue size, shape, or compactness, allowing it to recognize normal versus abnormal (for example, cancerous) tissues. Dermatologists currently use EIS through a device called Nevisense to track the effectiveness of melanoma treatments and to make decisions about whether questionable-looking bits of skin, like moles, should be excised or simply monitored. The Nevisense device generates a number from 0 to 10. A 0 to 3 means the lesion will be monitored over time and a 7-10 means it will immediately be excised as it is likely cancerous. Anything that falls in between is monitored until something changes, at which point it is often excised. This takes much of the guesswork out of identifying cancerous skin, can prevent the need for biopsies, and can save time by allowing for the immediate use of treatments instead of waiting for biopsy results.
EIS is also useful in other areas of the body. A variety of clinical trials are in various stages of completion to test EIS for a surprising range of potential applications. One clinical trial recently finished and published results showing that EIS could effectively distinguish tissues in the neck that are often difficult to tell apart during surgery. Two others that are currently recruiting will aim to test EIS for diagnosing esophageal cancer without performing a biopsy and to predict preterm childbirth.
When it came to determining the suitability of EIS for assessing skin barrier function, the researchers had to address two questions. First, would the instrument measure a greater resistance from healthy skin than it would from unhealthy skin? Second, would it perform as well, if not better, than the current TEWL method?
These questions were answered by artificially disrupting mouse skin and comparing it to mice with normal skin. The device requires bare skin, so the researchers used a hair removal cream and then waited three days to ensure that the cream application would not affect results. Researchers disrupted skin in a few ways, including several enzymes which would disrupt the interactions between cells, and "tape stripping," in which a piece of tape is repeatedly applied to the skin and ripped off to create irritation and break the skin barrier. Compared to normal mice, EIS measured less resistance from artificially disrupted mouse skin. This was the case for all methods used to disrupt skin barriers, suggesting that EIS measurements could differentiate between intact and disrupted skin barriers. As a comparison, the researchers also measured TEWL under the same conditions. Importantly, TEWL measurements mirrored the EIS data.
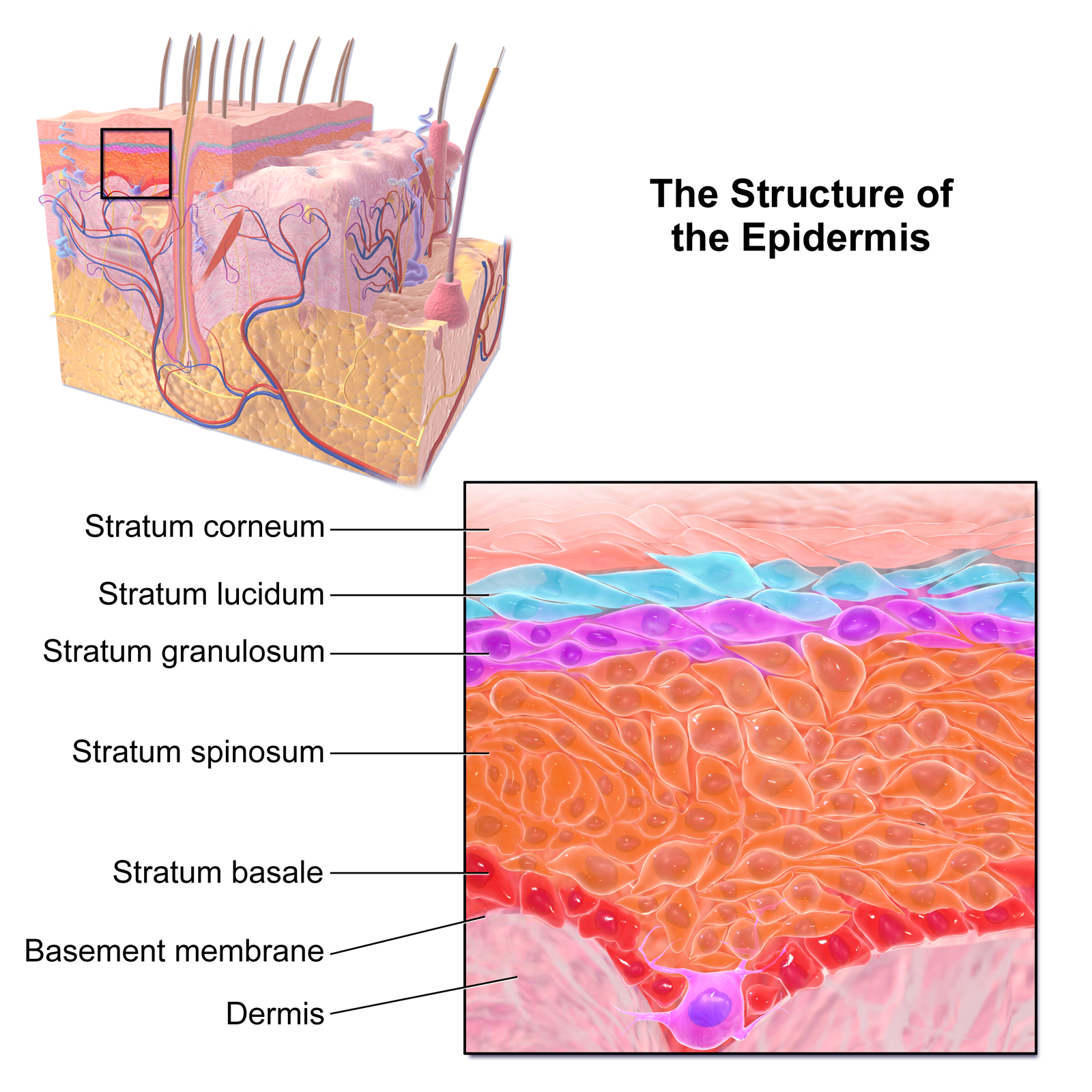
A diagram showing different layers of the epidermis.
Via Wikimedia
But the researchers also found that EIS could do something that TEWL could not. Skin is composed of three layers; the top layer that we see is the epidermis and is, itself, composed of four layers. Every layer of the epidermis has its own characteristics and purpose that is important for the overall function of the skin. These purposes are regulated by different sets of proteins. But this also means that skin disruption can originate from any individual layer. The 225 minuscule pins in the device’s ultrasensitive electrode are of different lengths, which allows the electric currents to pass through four different tissue depths and measure resistance at each of those depths. By recognizing one layer from another with EIS, it may be possible to identify both that the skin barrier is damaged and in which layer the damage exists, providing a greater understanding of an individual’s skin. Using this concept, the researchers found that both superficial and deep skin layers were less resistant to EIS than control skin, but this was more pronounced in the superficial layers.
The techniques used to artificially disrupt the mouse skin barrier are expected to disturb the superficial layers to a greater extent, suggesting that EIS can differentiate between these layers. Being able to identify the layer in which a skin barrier defect originates can potentially help determine the cause of the defect, not just for eczema, whose cause is unknown, but also for other skin disorders, opening up new avenues for patients, doctors, and scientists alike.
This newfound ability of EIS to measure differences in skin barrier function is extremely exciting. A clinical trial in Switzerland is currently recruiting individuals with or without eczema to test EIS on human skin. If found applicable, the device would have a variety of new, important uses. At-risk infants, such as those with family history, can be tested and preventative measures put in place before they start to show symptoms of eczema. For those who already have eczema, EIS could be used to track treatment efficacy. Beyond eczema, many skin disorders are caused by defective skin barriers, thus making EIS potentially applicable to those individuals as well.
