

Produced in partnership with NPR Scicommers
Can the right microbes really solve all your health problems?
A microbiologist explains the latest gut science
In addition to being delicious, kombucha, kimchi and yogurt all have something in common: they are all teeming with microorganisms. This sounds like a bad thing. However, by studying the microbiome, the collection of microbes that live on and inside our body, we’ve discovered that many bacteria are good for health – and some are, in fact, essential.
What started as a theory in the 1930s has, since genome sequencing became accessible, turned into a powerhouse of research establishing a link between our microbiome and health. This has led to a new wave of health products that contain “beneficial” microbes, also known as probiotics, supposedly to help prevent or cure illnesses.
But are any of these fads backed by real science? The short answer is no. The long answer, however, is a lot more interesting. There is now compelling evidence to suggest that our microbiome impacts the onset and severity of a range of diseases. No microbe can single-handedly cure a disease, but treatments targeted at nurturing or restoring a healthy microbial community hold great promise for improving the quality of our lives.
Our body is made up of approximately 10 trillion human cells and a slightly higher number of bacteria. These bacteria are not unwanted tenants, though. They help us digest food, boost our immunity, and ward off pathogens, and they affect everything in our body from the gut to the brain. As a collective group, they are as vital as the organs in our body. With advances in DNA sequencing technology in the past 20 years, we can now identify every member of this crucial microbial community.
Each one of us has a community of microbes that is unique to us, like a microbial fingerprint. The relationship between humans and the microbiome is mutually beneficial and has been millions of years in the making. Surprisingly, however, we haven’t found any bacteria that are universally present in all humans – different and unrelated microbes can perform similar functions in the human body, but there are patterns discernible within this diversity, and researchers have started to harness them to learn more about illness.
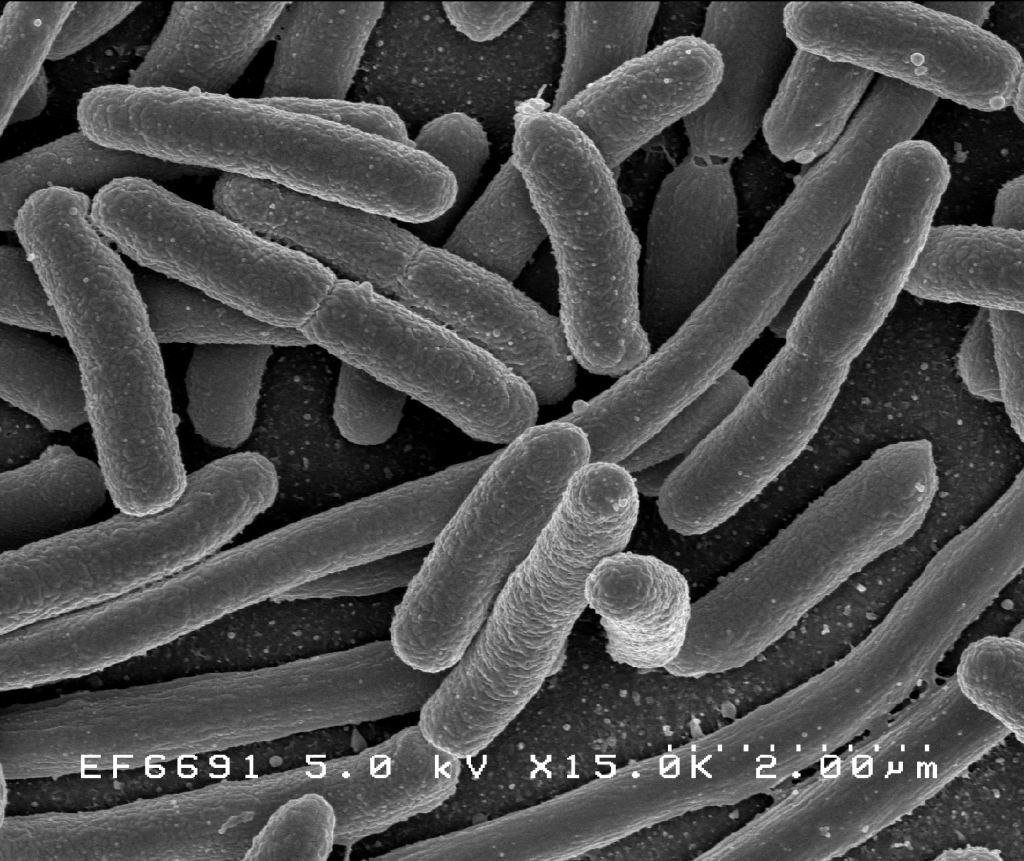
Escherichia coli, a bacteria commonly found in human gut flora
The genes collectively present in these microbes, unlike the static set of genes our bodies possess, are continuously changing. In response to variations in our diet and lifestyle, our microbes adapt and evolve at a pace that human cells never could. This pliability of the microbiome has tremendous potential: correcting a fault in the human genome is laborious and difficult. But a fault in our microbial community can theoretically be corrected much more easily.
Individuals suffering from obesity, irritable bowel syndrome, and even neurological disorders have a microbiome that is very different from healthy people. Can we identify good bacteria that are missing and reintroduce them into these patients to help restore health?
Having a drink filled with beneficial bacteria sounds simple enough. But how do we know that a bacterium is beneficial? Yes, there are bacteria present in healthy individuals that are reduced or missing during disease. But all that tells us is correlation; we don’t know whether their absence is the cause of the disease or just a consequence. The million-dollar question is whether a change in your microbial community can actually cause a disease. If the answer is 'yes,' then, like any other self-respecting pathogen, exposure to this imbalanced community should cause disease symptoms in a healthy person.
By making use of completely sterile animals, scientists are addressing this question. In the case of obesity, studies suggest that when lean animals are exposed to the gut microbes from an obese person they put on weight. Understanding the mechanism behind this can give us clues about how to design therapies that restore healthy microbial communities.
Interventions to nurture healthy microbes is not a concept we invented. Breast milk is the original, all-natural way to promote the growth of good bacteria. Breast milk contains hundreds of sugar molecules which the baby cannot digest. Instead, these sugars are fodder for specific bacteria in the baby’s gut. The milk shapes a microbial community that can train and protect the immune system of the baby. Interestingly, it is not the microbes alone but rather their behavior while digesting milk that makes them protective. Whether a bacterium is beneficial or not depends on the context of diet and environment.
In the body, microbes exist in mixed communities where they compete and cooperate with each other. This communal behavior endows humans with the ability to deal with changing diets, drug exposures as well as pathogen invasion. In the case of intractable infections such as Clostridium difficile (C. diff), the most effective therapy to date is transferring the microbes in the feces of a healthy donor to the patient. This fecal transplant restores a healthy microbial community capable of fighting the infection.
Rather than a single bacterial magic bullet, imagine instead a future that involves microbial concoctions tailor-made to your microbiome fingerprint to help restore equilibrium. Once we are able to understand and predict the consequences of manipulating our microbes, we will be able to harness their full therapeutic potential.
