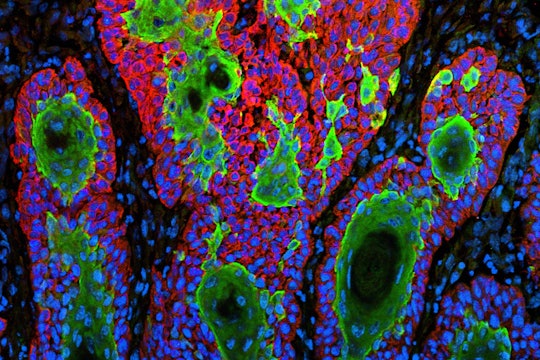
NIH Image Gallery / Flickr
To better target cancer, scientists find clues on the surface of cells
New research finds that we might need to take a step back from the inside of cells
Amongst all the wars waged throughout history, the war against cancer is perhaps one of the costliest; from the loss of loved ones and emotional distress caused by the disease, to the price of research and treatment itself. So, how far have we moved from the trenches? As researchers continue to probe into the workings of cancer, one thing is becoming clear: Performing targeted therapies against cancer-causing “onco”-genes is of utmost necessity if we are to have a fighting chance to overpower the malady.
To date, many of these genes still remain difficult drug targets, but scientists may just have stumbled upon a new approach that could potentially make it easier to find and fight these cancer-causing cells.
Our bodies contain various types of genes, known as proto-oncogenes, which make sure that all cells grow and multiply properly. When these genes mutate or multiply too much in the body, they are termed oncogenes (“onco-” relating to tumors) and can cause cells to divide uncontrollably and become cancerous. A 2004 census indicates that mutations in approximately one percent of human genes contribute to forming cancers. Due to this critical feature, oncogenes are a vital area of cancer research, and a target for anti-cancer drug design.
The 'worst' and the 'undruggable'
Out of the myriad known oncogenes, RAS is a particularly notorious one. The mutated, cancer-causing version of RAS genes was discovered in 1982, and 30 years on, is amongst the most frequently mutated gene in human cancers. Cited to be the “worst oncogene,” mutated forms of RAS are found in 60 to 90 percent of pancreatic cancer and are also prevalent in colorectal and lung cancers. The protein form of RAS lies on the surface of cells, acting as a major communication hub by interacting with the outside environment (such as other cells or molecules), and sending essential information into the cell.
Although vast progress has been made in understanding the involvement of RAS mutations in the development of cancer at a molecular level, there remains a cause for concern. RAS genes play an integral role in cell growth, division, and migration of healthy cells, and targeting them during cancer treatment could also have gross detrimental effects on normal cells. As a result, RAS oncogenes are largely considered “undruggable,” and in 2013, the National Institutes of Health launched the RAS Initiative specifically aimed to innovate and develop technologies to target this undruggable status.
To date, most researchers have studied how oncogenes cause cancer by looking at changes inside cancer cells. Biologist Alexander Martinko and colleagues at the University of California, San Francisco and Frederick National Laboratory for Cancer Research, however, did the opposite: They looked at changes caused by oncogenes on the outside, i.e., on the surface, of the cell, where numerous proteins such as Ras enable proper communication between the outside environment and the inside of cells.
In an effort to more directly target RAS, Martinko and his colleagues — working as part of the NIH initiative — studied the surface of cancer cells that had the RAS mutation to identify a specific protein “signature.” Specifically, they asked the question: Are there higher or lower levels of certain cell-surface proteins in RAS-driven cancer cells compared to normal ones? The team hoped that if this was the case, then targeting these abnormal proteins could be a means to identify RAS-derived cancer cells, and more effectively craft cancer-specific, individual treatment.
Previous research has shown that among all RAS-driven cancers, the most frequently mutated gene is KRAS. So, the researchers first generated cancerous skin cells with the KRAS mutation. These cells were then analyzed to identify and quantify the types of proteins present on the cell surface. Over 30 proteins were found to have significantly altered levels (either overabundant or reduced) in the presence of KRAS, with many necessary for cell movement and adhesion. To validate that the profile of the proteins seen on the surface of the cancer cells was due to the mutation and improper signals sent by the K-Ras protein, the cells were treated with molecules that inhibit K-Ras (spelled using lowercase and a hyphen to distinguish the protein from the gene). The researchers found that the K-Ras inhibitor enabled the altered proteins to return to normal levels, suggesting that the KRAS oncogene was indeed the cause of the altered protein levels.
Seeing that RAS mutations are common in pancreatic, lung, and colorectal cancers, cells from each of these cancer types were also tested for their cell surface protein profiles. Researchers noted that one of the proteins, CUB Domain Containing Protein 1 (CDCP1), stood out during all the tests, being the only protein that was observed to be in all the cancer types. They also found that CDCP1, previously known to be involved in tumor progression and metastasis, is increased in cancer cells harboring KRAS mutations.
Since higher CDCP1 levels could potentially act as a marker for cells with KRAS mutations, the research team used CDCP1 to selectively send anticancer drugs to the cancer cells with the KRAS mutations. They linked monomethyl auristatin F (MMAF, a synthetic anti-cancer drug) with a molecular marker that could identify and attach to the CDCP1 protein, and treated cancer cells. The MMAF-marker combination successfully introduced the drug into the KRAS cancer cells, killing more than 60 percent of these cells. The scientists published their results in the open access, peer-reviewed journal eLife in February.
The study presents “a novel technological pipeline for the discovery and application of antibodies to surface proteins regulated by cancer-causing signaling pathways,” molecular biologist James Wells, co-author of the new report, said in a statement. "This pipeline can be used to attack undruggable targets, including RAS, from the outside.”
The research offers an intriguing approach to the seemingly intractable problem of dismantling oncogenes that are also critical for normal cellular function. Using relatively modest techniques, proteins on the surface of cancer cells could be the secret operatives we needed all along, by acting as both distinct markers of cancer, and possible anti-cancer drug targets.The scientists' latest findings offer a new view of cancer, from the outside in.


Really enjoyed this piece. Gives another great perspective on how cancer is being tackled from so many angles.
I think it’s important to highlight the sentiment behind the terms druggable and undruggable to understand the context behind advances like these.
To me, undruggable means that we just haven’t found a way to drug them through conventional, practical mean that would make it administrable, safe, deliverable – all the things beyond “does it work?” that need to be in place for the therapy to reach patients.
Pharmaceutical companies are interested in all different ways to tackle these undruggable targets, like small peptides, monoclonal antibodies, nanobodies, chimeric antibodies, peptibodies, oncolytic viruses, antibody-drug conjugates, RNAi… So many avenues to investigate but just too much risk for large investments. In my opinion, this is where studies like these, that offer new and additional ways to identify, investigate, derisk cancer attack strategies, practically and positively impact the pipeline of the field.
And since surface markers have been so successful in the past, I’m excited to see how this work gets translated beyond the journal.